by Eric Cressey
Today's guest post comes from Physical Therapist Chris Leib. Enjoy! -EC
Recently, there has been plenty of discussion regarding the efficacy of the idea of posture and whether attempting to improve it is a useful tactic for decreasing pain. This discussion has been perpetuated by research indicating that there is a surprisingly poor correlation between pain and posture. The evidence seems to be pretty damning on this topic, which raises questions about whether looking at pain as an outcome measure actually makes sense when discussing posture. Moreover, even more basic questions still need to be asked regarding the very definition of posture.
When discussing these inquiries, it’s important to understand that the current research has demonstrated that pain is far more complex than previously thought, and that a single model of physiological stress will not be sufficient to demonstrate why some people experience pain and some do not. A discussion of pain science is too complicated to be brushed over in the present discussion; however, it must be understood:
Just because proper posture hasn’t been highly correlated with pain doesn’t mean it’s not important.
When looking deeper into the studies cited above, it becomes clear that there is not a consensus definition of posture. Instead of looking at the constantly changing nature of posture, many of these studies defined posture by using various markers of static structure. Taking this fact into consideration, one must ask the following question: If no agreement is reached as to what proper posture is, how can it be well studied?
In my experience over the past decade as both a strength and conditioning professional and physical therapist, my own definition of proper posture has evolved considerably. Utilizing these years of clinical experience and the current research, I would like to set forth the following 4 Rules of Posture.
Rule #1: Posture May Not Cause Pain, But Improving Posture Can Help to Decrease Pain.
Although there is poor evidence that various definitions of poor posture are associated with increased pain, it’s obvious through clinical assessment that a change in posture can decrease pain when it is present. Go to any physical therapy clinic and you will find patients in pain getting education regarding postural changes that improve their symptoms on the spot. Pain can be a great indicator of what the body feels is a stable position. Often, immediate positive changes are made just by getting the person into a different position.
A common example is the individual with neck pain who has pain when sitting slouched with his or her head forward. Frequently, a combination of education and ergonomic adjustment can abolish this excruciating pain in shorter order. Now, this isn’t to say that the quick fix always “cures” the problem, but it does gives the person more feelings of control over making change with regard to their pain, which actually goes a long way. This sense of control has been demonstrated to be a positive indicator of recovery from and the ability to cope with chronic pain .
Rule #1 is the only rule in which we’ll discuss pain. As I noted, the research on pain indicates that the science is far too complex to discuss isolated associations. Clinically, pain can be a good feedback indicator of postures and positions that a person’s body finds unsafe. This feedback helps determine the best positions for the person to train in and, with time, adopt.
The subsequent three rules will discuss posture in relation to functional and physical performance-based movement quality.
Rule #2: Support Yourself Actively and Passively.
This rule will illustrate the difference between passive and active postural stability, as well as the appropriate balance that’s needed between the two. Let’s get some definitions out of the way first.
Generally speaking, passive stability is using something other than balanced muscular effort to adopt and maintain a desired position. Passive stability can either be anatomical or external in nature. Anatomical passive stability utilizes one’s passive stability structures such as joint capsules, cartilage, and ligaments to find stability in a position, while external passive stability utilizes an external item for extra support when attempting to maintain a position. When dealing with passive stability of any type, the common denominator is finding a stable position while decreasing relative muscular effort.
Active postural stability, on the other hand, refers to the use of muscles to maintain a desired position. In order to optimize muscle activity during static and dynamic postures, the attachments of the muscles must be positioned so that the muscles contract in a balanced way. In addition, the position should minimize energy expenditure against the pull of gravity.
For clarification on how best to determine optimal positioning based on the above definitions, let’s illustrate a common static and dynamic example.
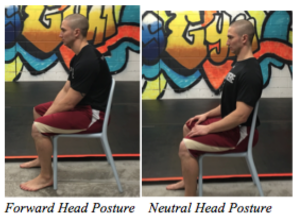
i. Static postural stability: Sitting in a chair
No matter what, this common static position will never be ideal for postural stability due to the severe muscle imbalances inherent to sitting with your hips and knees in 90 degrees of flexion. However, sitting with the head and shoulders substantially in front of the line of gravity makes a bad situation even worse. The further forward the head and shoulders travel out in front of this line, the more effort the muscles that hold up the head and trunk must exert. More importantly, because the muscles in this case are overstretched and in a poor position to function in a balanced way, less resilient structures such as ligaments and joint capsules/cartilages are forced to pick up the slack.
Thus, the most optimal default position in sitting is the one that minimizes the effort of your muscles and stress to your other more passive structures by allowing the head and shoulders to balance effortlessly in the line of gravity. (Feel free to take this opportunity to observe your own posture. Are your head and shoulders neatly stacked or forward like the pass from the 2000 Music City Miracle?)
ii. Dynamic postural stability: Deadlifting a heavy load from the ground
In this dynamic example, the muscles of the hips, lower back, abdomen, and thorax will be in the most balanced position to lift the load when the pelvis is in a neutral position. That is to say, the lower back should neither be flexed nor extended. In this position, the muscles of the lower back are well balanced with that of the abdomen, and the hip extensors have a better opportunity to contract during the lift.
If the lift were initiated with the lower spine in an extended position, the position can still indeed be stable; however, the stability would come from passive anatomical structures such as the lumbar facet joints and ligaments of the anterior spine. This position increases compressive forces to the lower back and decreases the contractile ability of both the abdominals and hip extensors, as both of these muscle groups are now in an over-lengthened position.
Therefore, the optimal position for the dynamic movement of deadlifting is the one that allows for the hip/trunk flexors and hip/trunk extensors to work in the most balanced fashion (see video below). Moreover, setting up the movement and transitioning the bar in such a way that the load stays as close to the body as possible minimizes the downward pulling effects from gravity much like the head and shoulders staying over the midline of the body in the previous sitting example.
When attempting to understand how best to balance active and passive stability within a specific task, we must take into consideration four factors: (1) the available tissue mobility in order to get into the position required; (2) the external objects manipulated or used for positioning; (3) the duration of the task; (4) the intensity of the task.
Let’s return once again to our two examples:
i. Static postural stability: Sitting in a chair
For static sitting, we must first assess ranges of motion like thoracic extension, shoulder internal/external rotation, and scapular retraction/depression/posterior tilt. In doing so, we’re able to determine whether the desired position can be assumed without pain or excessive compensatory muscle effort. Moreover, we must know the type of seat the client will be utilizing and what activities he or she will be doing while sitting (i.e. typing, driving, etc.).
In terms of duration and intensity, sitting will typically fall under the category of a low intensity activity done for long durations. The longer the duration, the more muscular endurance necessary to maintain a desired position. If any of the above factors are not optimal, external passive support in the form of a lumbar cushion, posture shirt, or corrective tape may be necessary to enable the client to attain a more favorable posture without excessive effort.
(Passively elevating the hips to decrease the effort to maintain an upright torso)
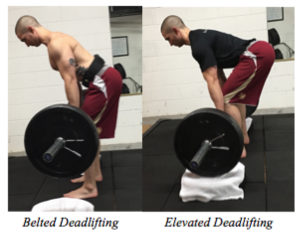
ii. Dynamic postural stability: Deadlifting a heavy load from the ground
With deadlifting, mobility limitations in the hips and trunk can often limit an individual’s ability to adopt and maintain the optimal stable position described above. In addition, the intensity of the load or duration of the set must not exceed the amount of muscular force the individual is able to generate, or else even a solid initial position will be lost.
In cases where mobility restrictions are a limiting factor, passive support can come in the form of apparatuses that decrease the range of motion of the movement (i.e. elevating the load onto blocks or a rack). When approaching maximal loads or durations, passive support may take the form of stability belts and braces in areas most susceptible to positional failure.
3. Posture is the Product of Your Movement Variability.
Posture is often discussed as a single static element that represents one’s lack of mindfulness or genetic misfortune. Clinical experience and the current scientific literature say this belief is not only wrong, but also a harmful notion to the process of making postural change. One shouldn’t feel guilty or unfortunate that he or she is demonstrating an unskillful posture. Instead, there should be an understanding that posture is not a single static entity, but rather task dependent and constantly changing.
The secret to good posture is that you shouldn’t need to work for it when you are at rest. You see, your static postures during sitting, standing, and walking are a product of your cumulative movement throughout the day. Our bodies are built to adapt to the positions and activities we take on most frequently. If any of these positions and activities are done is excess, all our positions and movement can become imbalanced. This imbalance is what is deemed by many as poor posture, but in reality it is just the body doing what it does best: adapting.
In order to prevent postural imbalances, it is unwise to attempt to simply make ergonomic adjustments to the positions we sustain too frequently. Instead, we must consider our whole body of movement throughout the day. If we focus on proper positioning in training, it will inevitably transfer to our static postures. In this way, programming for any strength, conditioning, or fitness routine must involve a strong focus on developing positions that promote muscular balance (active postural stability) and task transference, as opposed to simply task completion.
For example, there are many ways to push yourself up from the ground when doing a push-up, but there are positioning subtleties that can either promote balanced muscular stability or feed habits of chronic positioning that we already practice too frequently throughout the day (see video below). Thus, an individual’s movement practice should be about movement quality and variability as much as about cultivating strength and conditioning.
Mindless prescription of physical activity (i.e. 30-60 minutes of aerobic exercises; 3 sets of 10 of machine based resistance exercise) prioritizes strength and conditioning capacity over movement capability and variability, hoping that by blindly improving one’s quantity of routine movements the quality of movement will also improve. Don’t get me wrong, in moderation, more movement is better than less movement. However, too much of the same movements can create similar problems as too little movement.
4. Counterbalance Your Life.
The idea of increasing movement quality and variability goes way beyond one’s time at the gym. To allow for increased ease of active postural stability, the common patterns of one’s entire day need to be understood so that behavioral change can be implemented. This is not to say that if we sit all day at work then we need to get a new job. That’s just not practical. Nor does it mean that we must be obsessed with maintaining an upright posture or “drawing our abdomens in” all day long. It simply calls for awareness — awareness of the positions that are most frequently adopted and strategies for counterbalancing them.
Guidelines for this awareness are three-fold:
i. Understand the chronic positions you adopt.
Often postural counterbalances are subtle and developing improved body awareness becomes much more important than simply adjusting your position. This improved body education can come in many forms, such as independent reading on anatomy and physiology, advice from a movement professional, or cultivation of a versatile movement practice as discussed above. It’s important to know that ultimately YOU have the best opportunity to understand your own body. It can be a gradual process to refine this body awareness, but once developed, understanding the positions and movements that are healthy versus harmful to your specific body becomes much easier.
ii. Separate times you must be stationary and times you choose to be stationary.
It’s important to have a plan of attack for positioning throughout your day. Practically speaking, if you sit all day at work, acknowledge it, and then minimize the time you sit when in the comfort of your home. Likewise, if you are on your feet all day, don’t be afraid to spend some time vegging out on the couch. One stationary position is not necessarily better than the other (i.e. standing is not better than sitting). It’s the one that you do most frequently that will usually lead to problems.
iii. Expand your positional repertoire.
When attempting to adopt positions different from those in which you are most comfortable, it is important to have other positions at your disposal. For example, sitting in a chair is a completely different mechanical stress than sitting cross-legged on the ground, just as standing stationary on two legs is different than weight shifting effortlessly from one leg to the other. Similar to the idea of developing more movement variability in an exercise practice, it’s important that you’re able to adopt positions besides those you do most frequently. This may be another area where the help of a movement professional is necessary so that you can become comfortable with the mobility and stability necessary to adopt different variations of sitting and standing positions.
See the video playlist below regarding positional variations for sitting (chair and ground) and standing:
In conclusion, there is plenty of disagreement and misunderstanding around the topic of posture. In my experience, this controversy is unnecessary and overblown. Any respectable strength and conditioning professional would agree that proper positioning and technique is vital when undertaking various movements in a strength and conditioning program. Why should the importance of positioning be any different in our movements throughout the day? We must understand that our bodies are constantly changing; therefore, posture should be viewed as a dynamic, ever-changing journey — not a fixed destination. Hopefully the 4 Rules of Posture set forth above allow you to better understand how to embrace this journey!
About the Author
Chris Leib of MovementProfessional.com is a licensed Doctor of Physical Therapy and Certified Strength and Conditioning Specialist with nearly a decade of experience in treating movement dysfunctions and enhancing human performance. He has written for many popular training and rehabilitation websites, and has a versatile movement background with a variety of certifications as both a physical therapist and fitness professional. Chris considers physical activity a vital process to being a complete human being and is passionate about helping others maximize their movement potential. Be sure to follow him on Facebook and YouTube.
Chris Leib of MovementProfessional.com is a licensed Doctor of Physical Therapy and Certified Strength and Conditioning Specialist with nearly a decade of experience in treating movement dysfunctions and enhancing human performance. He has written for many popular training and rehabilitation websites, and has a versatile movement background with a variety of certifications as both a physical therapist and fitness professional. Chris considers physical activity a vital process to being a complete human being and is passionate about helping others maximize their movement potential. Be sure to follow him on Facebook and YouTube.
A special thanks to Travis Pollen of www.FitnessPollenator.com for his help with this article.
References
1. Grundy, Roberts (1984) Does unequal leg length cause back pain? A case-control study. Lancet. 1984 Aug 4;2(8397):256-8. http://www.ncbi.nlm.nih.gov/pubmed/6146810
2. Pope, M., Bevins, T., Wilder, D., & Frymoyer, J. (1985). The Relationship Between Anthropometric, Postural, Muscular, and Mobility Characteristics of Males Ages 18-55. Spine, 644-648. http://www.ncbi.nlm.nih.gov/pubmed/4071274
3. Grob, D., Frauenfelder, H., & Mannion, A. (2006). The association between cervical spine curvature and neck pain. European Spine Journal Eur Spine J, 669-678. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2213543/
4. Nourbakhsh, M., & Arab, A. (2002). Relationship Between Mechanical Factors and Incidence of Low Back Pain. J Orthop Sports Phys Ther Journal of Orthopaedic & Sports Physical Therapy, 447-460. http://www.ncbi.nlm.nih.gov/pubmed/12322811
5. Dieck, G., Kelsey, J., Goel, V., Panjabi, M., Walter, S., & Laprade, M. (1985). An Epidemiologic Study of the Relationship Between Postural Asymmetry in the Teen Years and Subsequent Back and Neck Pain. Spine, 872-877. http://www.ncbi.nlm.nih.gov/pubmed/2938272
6. Franklin, M., & Conner-Kerr, T. (1988). An Analysis of Posture and Back Pain in the First and Third Trimesters of Pregnancy. J Orthop Sports Phys Ther Journal of Orthopaedic & Sports Physical Therapy, 133-138. http://www.ncbi.nlm.nih.gov/pubmed/9742469
7. Lederman, E. (2010). The fall of the postural-structural-biomechanical model in manual and physical therapies: Exemplified by lower back pain. Journal of Bodywork and Movement Therapies, 131-138. http://www.cpdo.net/Lederman_The_fall_of_the_postural-structural-biomechanical_model.pdf
8. Christensen, S., & Hartvigsen, J. (2008). Spinal Curves and Health: A Systematic Critical Review of the Epidemiological Literature Dealing With Associations Between Sagittal Spinal Curves and Health. Journal of Manipulative and Physiological Therapeutics, 690-714. http://www.ncbi.nlm.nih.gov/pubmed/19028253
9. Evidence-Base for Explain Pain, Second Edition. (n.d). Retrieved October 2, 2015. http://www.noigroup.com/documents/noi_explain_pain_2nd_edn_evidence_base_0813.pdf
2. Pope, M., Bevins, T., Wilder, D., & Frymoyer, J. (1985). The Relationship Between Anthropometric, Postural, Muscular, and Mobility Characteristics of Males Ages 18-55. Spine, 644-648. http://www.ncbi.nlm.nih.gov/pubmed/4071274
3. Grob, D., Frauenfelder, H., & Mannion, A. (2006). The association between cervical spine curvature and neck pain. European Spine Journal Eur Spine J, 669-678. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2213543/
4. Nourbakhsh, M., & Arab, A. (2002). Relationship Between Mechanical Factors and Incidence of Low Back Pain. J Orthop Sports Phys Ther Journal of Orthopaedic & Sports Physical Therapy, 447-460. http://www.ncbi.nlm.nih.gov/pubmed/12322811
5. Dieck, G., Kelsey, J., Goel, V., Panjabi, M., Walter, S., & Laprade, M. (1985). An Epidemiologic Study of the Relationship Between Postural Asymmetry in the Teen Years and Subsequent Back and Neck Pain. Spine, 872-877. http://www.ncbi.nlm.nih.gov/pubmed/2938272
6. Franklin, M., & Conner-Kerr, T. (1988). An Analysis of Posture and Back Pain in the First and Third Trimesters of Pregnancy. J Orthop Sports Phys Ther Journal of Orthopaedic & Sports Physical Therapy, 133-138. http://www.ncbi.nlm.nih.gov/pubmed/9742469
7. Lederman, E. (2010). The fall of the postural-structural-biomechanical model in manual and physical therapies: Exemplified by lower back pain. Journal of Bodywork and Movement Therapies, 131-138. http://www.cpdo.net/Lederman_The_fall_of_the_postural-structural-biomechanical_model.pdf
8. Christensen, S., & Hartvigsen, J. (2008). Spinal Curves and Health: A Systematic Critical Review of the Epidemiological Literature Dealing With Associations Between Sagittal Spinal Curves and Health. Journal of Manipulative and Physiological Therapeutics, 690-714. http://www.ncbi.nlm.nih.gov/pubmed/19028253
9. Evidence-Base for Explain Pain, Second Edition. (n.d). Retrieved October 2, 2015. http://www.noigroup.com/documents/noi_explain_pain_2nd_edn_evidence_base_0813.pdf
10. Control, culture and chronic pain. (n.d.). Retrieved October 2, 2015.
http://www.sciencedirect.com/science/article/pii/0277953694900205
http://www.sciencedirect.com/science/article/pii/0277953694900205
11. Garber, C., Blissmer, B., Deschenes, M., Franklin, B., Lamonte, M., Lee, I., Swain, D. (2011). Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults. Medicine & Science in Sports & Exercise, 1334-1359. http://journals.lww.com/acsm-msse/Fulltext/2011/07000/Quantity_and_Quality_of_Exercise_for_Developing.26.aspx

Комментариев нет:
Отправить комментарий